- Overview and Evaluation of Hand Disorders
- Boutonnière Deformity
- Carpal Tunnel Syndrome
- Cubital Tunnel Syndrome
- De Quervain Syndrome
- Trigger Finger (Stenosing Flexor Tenosynovitis)
- Dupuytren Contracture
- Felon
- Ganglia
- Herpetic Whitlow
- Infected Bite Wounds of the Hand
- Infectious Flexor Tenosynovitis
- Kienböck Disease
- Osteoarthritis of the Hand
- Palm Abscess
- Radial Tunnel Syndrome
- Swan-Neck Deformity
Topic Resources
Common hand disorders include a variety of deformities, ganglia, infections, Kienböck disease, nerve compression syndromes, noninfectious tenosynovitis, and osteoarthritis. (See also complex regional pain syndrome [reflex sympathetic dystrophy] and hand injuries.)
MEDICAL RF.COM/SCIENCE PHOTO LIBRARY
Hand deformities
Deformities of the hand can result from generalized disorders (eg, arthritis) or dislocations, fractures, and other localized disorders. Most nontraumatic localized disorders can be diagnosed by physical examination. Once a hand deformity becomes firmly established, it cannot be significantly altered by splinting, exercise, or other nonsurgical treatment.
Hand infections
Hand infections are typically classified as superficial or deep. Superficial infections involve the skin and subcutaneous tissues. Deep infections can involve the tendon sheaths, tendons, deep fascial planes, joint spaces, and bones. Untreated superficial hand infections can progress to deep infections. Prompt evaluation and treatment of a suspected hand infection is imperative to avoid severe infection and disability.
Common bacterial hand infections include paronychia, infected bite wounds, felon, palm abscess, and infectious flexor tenosynovitis. Herpetic whitlow is a viral hand infection. Infections often begin with constant, intense, throbbing pain and are usually diagnosed by physical examination. Radiographs are taken in some infections (eg, bite wounds, infectious flexor tenosynovitis) to detect occult foreign bodies but may not detect small or radiolucent objects. Blood cultures should be taken if a hematogenous source is suspected, and joint aspiration should be performed if septic arthritis is suspected.
Treatment of most hand infections involves surgical measures and antibiotics. The increased incidence of community-acquired and nosocomial methicillin-resistant Staphylococcus aureus (MRSA) should be taken into consideration (1). Uncomplicated MRSA infections are best treated with incision and drainage (2). If there is a high incidence of MRSA and the infection is severe, hospitalization for IV antibiotic therapy is recommended, as is consultation with an infectious disease specialist. For outpatients, trimethoprim/sulfamethoxazole, clindamycin, doxycycline, or linezolid (for oral therapy) can be given. Once culture and sensitivity results rule out MRSA, nafcillin, cloxacillin, dicloxacillin, or a first- or second-generation cephalosporin can be given. Nontuberculous mycobacterial infections should be considered in patients with more subacute inflammation, especially in those who are immunosuppressed./sulfamethoxazole, clindamycin, doxycycline, or linezolid (for oral therapy) can be given. Once culture and sensitivity results rule out MRSA, nafcillin, cloxacillin, dicloxacillin, or a first- or second-generation cephalosporin can be given. Nontuberculous mycobacterial infections should be considered in patients with more subacute inflammation, especially in those who are immunosuppressed.
Additional treatment measures include elevating the hand to help reduce edema and sometimes splinting.
Nerve compression syndromes of the hand
Common nerve compression syndromes include carpal tunnel syndrome, cubital tunnel syndrome, and radial tunnel syndrome. Compression of nerves often causes paresthesias; these paresthesias can often be reproduced by tapping the compressed nerve, usually with the examiner’s fingertip (Tinel sign). Suspected nerve compression can be confirmed by testing nerve conduction velocity and distal latencies, which accurately measure motor and sensory nerve conduction. Initial treatment is usually conservative (eg, rest, modified work environment, splinting, corticosteroid injection), but surgical decompression may be necessary if conservative measures fail or if there are significant motor or sensory deficits.
Noninfectious tenosynovitis
(See also Tendinitis and Tenosynovitis.)
Tenosynovitis may involve any of the tendons in or around the hand. Common conditions include digital flexor tendinitis and tenosynovitis (trigger finger) and De Quervain syndrome.
General references
1. O'Malley M, Fowler J, Ilyas AM: Community-acquired methicillin-resistant Staphylococcus aureus infections of the hand: Prevalence and timeliness of treatment. J Hand Surg Am 34(3):504–508, 2009. doi: 10.1016/j.jhsa.2008.11.021.
2. Chen WA, Plate JF, Li Z: Effect of setting of initial surgical drainage on outcome of finger infections. J Surg Orthop Adv 24(1):36–41, 2015. PMID: 25830261.
Evaluation of Hand Disorders
History and physical examination findings are often diagnostic in hand disorders.
History
The history should include information about any trauma or other events that may be associated with symptoms. The presence and duration of deformity and difficulty with motion are noted. The presence, duration, severity, and factors that exacerbate or relieve pain are elicited. Associated symptoms, such as fever, swelling, rashes, Raynaud syndrome, paresthesias, morning stiffness, other joint involvement, low back pain, and weakness, are also recorded.
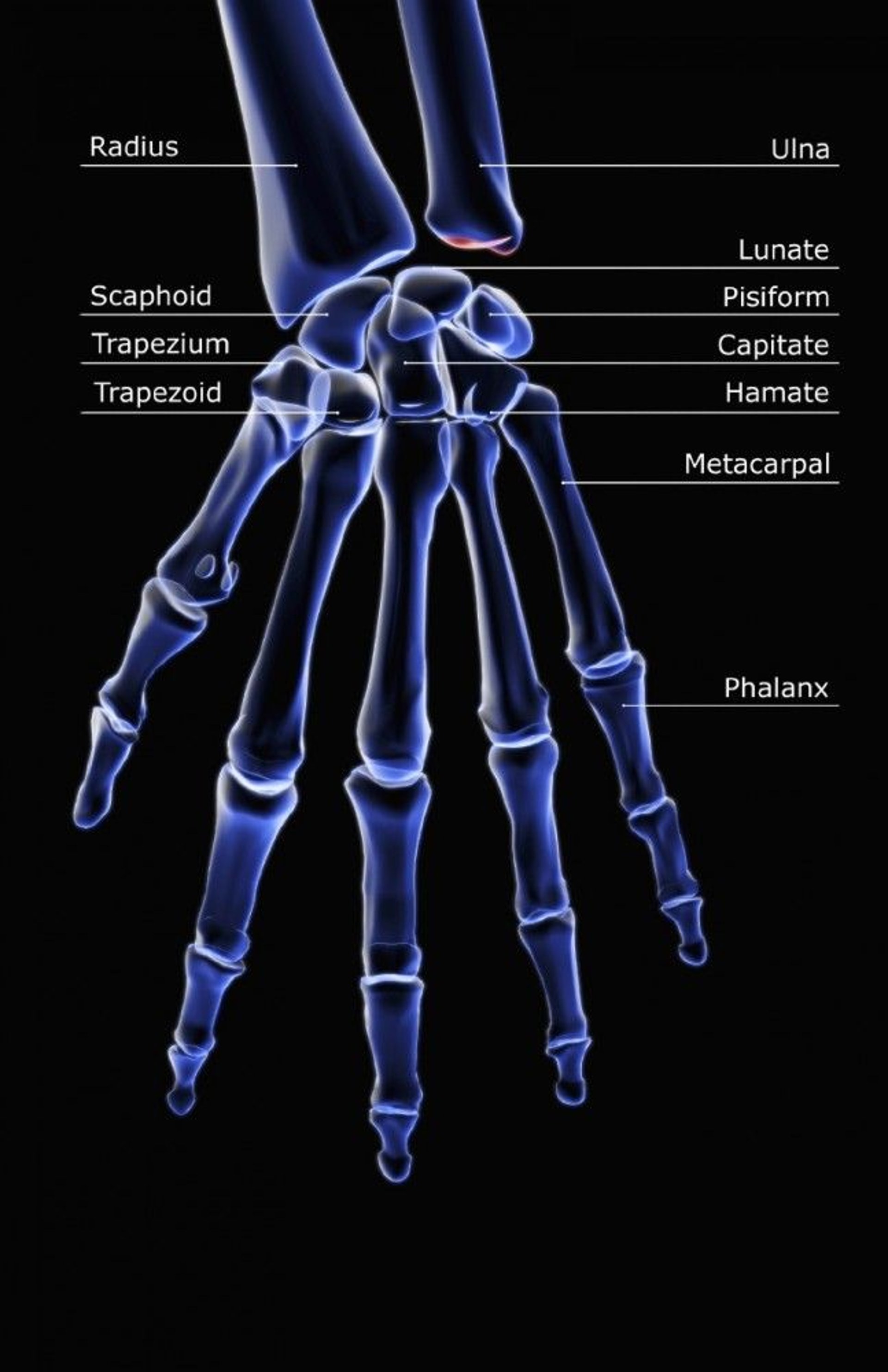
Physical examination
Examination should include inspection for erythema, swelling, or deformity and palpation for tenderness. Active range of motion should be tested for any possible tendon injury. Passive range of motion can detect the presence of fixed deformities and assess whether specific motions aggravate pain. Sensation may be tested by 2-point discrimination, using 2 ends of a paper clip. Motor function testing involves muscles innervated by the radial, median, and ulnar nerves. Vascular examination should include evaluation of capillary refill, radial and ulnar pulses, and the Allen test. Stress testing is helpful when specific ligament injuries are suspected (eg, ulnar collateral ligament in gamekeeper’s thumb). Provocative testing can aid in the diagnosis of tenosynovitis and nerve compression syndromes.
Testing
Laboratory testing can aid the diagnosis of inflammatory arthropathies (eg, rheumatoid arthritis) but otherwise has a limited role. Synovial fluid analysis remains the gold standard for definitive diagnosis of crystal-induced arthritides (eg, gout or calcium pyrophosphate arthritis) and infectious arthritis.
Ultrasound and dual-energy CT imaging may provide radiographic evidence of uric acid deposition in patients with suspected gout, particularly in cases where joint aspiration is not possible or was unsuccessful.
Radiographs and MRI are helpful for detecting injuries, some types of arthritis (eg, osteoarthritis, erosive rheumatoid arthritis), and Kienböck disease or to rule out hidden foreign bodies that could be sources of infections.
MRI and ultrasonography can help assess tendon structure and integrity and detect deep abscesses. High-resolution ultrasound allows imaging in real-time motion and is especially helpful for evaluating tendons and synovitis.
Nerve conduction testing can help diagnose nerve compression syndromes. MRI and ultrasound are alternative diagnostic tests that can confirm the presence of peripheral nerve compression, although they provide no direct information about nerve function (1-3).
Bone scan is an alternative to MRI for the diagnosis of occult fractures and may aid the diagnosis of complex regional pain syndrome.
Evaluation references
1. Park JS, Won HC, Oh JY, Kim DH, et al: Value of cross-sectional area of median nerve by MRI in carpal tunnel syndrome. Asian J Surg 43(6):654-659, 2020. doi: 10.1016/j.asjsur.2019.08.001. Epub 2019 Aug 28. PMID: 31473048.
2. Wiesler ER, Chloros GD, Cartwright MS, et al: Ultrasound in the diagnosis of ulnar neuropathy at the cubital tunnel. J Hand Surg Am 31(7):1088-93, 2006. doi: 10.1016/j.jhsa.2006.06.007. PMID: 16945708.
3. Fowler JR, Munsch M, Tosti R, et al: Comparison of ultrasound and electrodiagnostic testing for diagnosis of carpal tunnel syndrome: study using a validated clinical tool as the reference standard. J Bone Joint Surg Am 96(17):e148, 2014. doi: 10.2106/JBJS.M.01250. PMID: 25187592.