Autism spectrum disorder is a neurodevelopmental disorder characterized by impaired social interaction and communication, repetitive and stereotyped patterns of behavior, and uneven intellectual development often with intellectual disability. Symptoms begin in early childhood. The cause in most children is unknown, although evidence supports a genetic component; in some patients, the disorder may be associated with a medical condition. Diagnosis is based on developmental history and observation. Treatment consists of behavioral management and sometimes medication therapy.
Ресурси за темою
Autism spectrum disorder represents a range of neurodevelopmental differences and is considered a neurodevelopmental disorder.
Neurodevelopmental disorders are neurologically based conditions that appear early in childhood, typically before school entry, and affect development of personal, social, academic, and/or occupational functioning. They typically involve difficulties with the acquisition, retention, or application of specific skills or sets of information. Neurodevelopmental disorders may involve dysfunction in attention, memory, perception, language, problem-solving, or social interaction. Other common neurodevelopmental disorders include attention-deficit/hyperactivity disorder, learning disorders (eg, dyslexia), and intellectual disability.
Current estimates of prevalence of autism spectrum disorder are in the range of 1/36 (based on estimates of the prevalence of autism spectrum disorder among children aged 8 years) in the United States (1), with similar ranges in other countries. Autism spectrum disorder is approximately 4 times more common among boys. The number of cases of autism spectrum disorder diagnosed has increased, partially because of changes in diagnostic criteria.
Довідковий матеріал загального характеру
1. Maenner MJ, Shaw KA, Bakian AV, et al: Prevalence and Characteristics of Autism Spectrum Disorder Among Children Aged 8 Years - Autism and Developmental Disabilities Monitoring Network, 11 Sites, United States, 2018. MMWR Surveill Summ 70(11):1–16, 2021. Published 2021 Dec 3. doi:10.15585/mmwr.ss7011a1
Etiology of Autism Spectrum Disorder
The specific cause in most cases of autism spectrum disorder remains elusive. However, some cases have occurred with congenital rubella syndrome, cytomegalic inclusion disease, phenylketonuria, tuberous sclerosis complex, or Fragile X syndrome.
Strong evidence supports a genetic component (1). For parents of one child with autism spectrum disorder, risk of having a subsequent child with autism spectrum disorder is around 5 to 10% (2). The risk is higher (approximately 7%) if the affected child is a female and lower (approximately 4%) if the affected child is a male (3). The concordance rate of autism is high in monozygotic twins. Research on families has suggested several potential target gene areas, including those related to neurotransmitter receptors (serotonin and gamma-aminobutyric acid [GABA]) and central nervous system structural control (HOX genes).
Environmental causes have been suspected but are unproved. There is compelling evidencethat vaccinations do not cause autism, and the primary study that suggested this association was withdrawn because its author falsified data (see also Measles-mumps-rubella (MMR) vaccine).
Differences in brain structure and function probably underlie much of the etiology of autism spectrum disorder. Differences have been identified in the cerebellum, amygdala, hippocampus, frontal cortex, and brain stem nuclei (4).
Research also suggests incidence of autism spectrum disorder increases with increasing prematurity (5).
Довідкові матеріали щодо етіології
1. Hyman SL, Levy SE, Myers SM; COUNCIL ON CHILDREN WITH DISABILITIES, SECTION ON DEVELOPMENTAL AND BEHAVIORAL PEDIATRICS: Identification, Evaluation, and Management of Children With Autism Spectrum Disorder. Pediatrics 145(1):e20193447, 2020. doi:10.1542/peds.2019-3447
2. Hansen SN, Schendel DE, Francis RW, et al: Recurrence Risk of Autism in Siblings and Cousins: A Multinational, Population-Based Study. J Am Acad Child Adolesc Psychiatry 58(9):866–875, 2019. doi:10.1016/j.jaac.2018.11.017
3. Palmer N, Beam A, Agniel D, et al: Association of Sex With Recurrence of Autism Spectrum Disorder Among Siblings. JAMA Pediatr 171(11):1107–1112, 2017. doi:10.1001/jamapediatrics.2017.2832
4. Donovan APA, Basson MA: The neuroanatomy of autism—A developmental perspective. J Anat 230(1): 4–15, 2017. doi: 10.1111/joa.12542
5. Crump C, Sundquist J, Sundquist K: Preterm or early term birth and risk of autism. Pediatrics 148(3):e2020032300, 2021. doi: 10.1542/peds.2020-032300
Symptoms and Signs of Autism Spectrum Disorder
Autism spectrum disorder may manifest during the first year of life, but, depending on severity of symptoms, diagnosis may not be clear until school age.
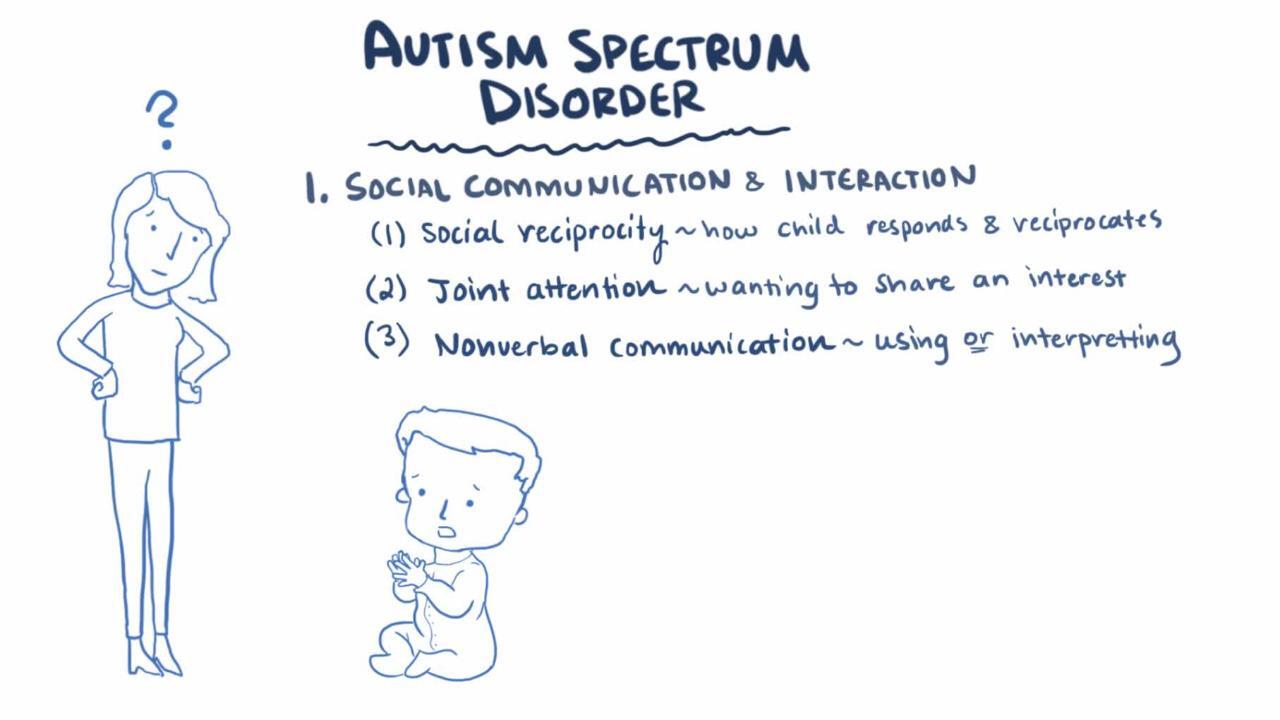
Two main features characterize autism spectrum disorder:
Persistent deficits in social communication and interaction
Restricted, repetitive patterns of behavior, interests, and/or activities
Both of these features must be present at a young age (although they may not be recognized at the time) and must be severe enough to significantly impair the child's ability to function at home, school, or other situations. Manifestations must be more pronounced than expected for the child’s developmental level and adjusted for norms in different cultures.
Examples of deficits in social communication and interaction include
Deficits in social and/or emotional reciprocity (eg, failure to initiate or respond to social interactions or conversation, no sharing of emotions)
Deficits in nonverbal social communication (eg, difficulty interpreting others' body language, gestures, and expressions; diminished facial expressions and gestures and/or eye contact)
Deficits in developing and maintaining relationships (eg, making friends, adjusting behavior to different situations)
The first manifestations noticed by parents may be delayed language development, lack of pointing at things from a distance after age 15 months, and lack of interest in parents or typical play.
Examples of restricted, repetitive patterns of behavior, interests, and/or activities include
Stereotyped or repetitive movements or speech (eg, repeated hand flapping or finger flicking, repeating idiosyncratic phrases or echolalia, lining up toys)
Inflexible adherence to routines and/or rituals (eg, having extreme distress with small changes in meals or clothing, having stereotyped greeting rituals)
Highly restricted, abnormally intense, fixated interests (eg, preoccupation with vacuum cleaners)
Extreme over- or under-reaction to sensory input (eg, extreme aversion to specific smells, tastes, or textures; apparent indifference to pain or temperature)
Some affected children injure themselves. Approximately 25% of affected children experience a documented loss of previously acquired skills (1).
All children with autism spectrum disorder have at least some difficulty with interaction, behavior, and communication; however, the severity of the problems varies widely.
One commonly held current theory holds that a fundamental problem in autism spectrum disorder is "mind blindness," the inability to imagine what another person might be thinking. This difficulty is thought to result in interaction abnormalities that, in turn, lead to abnormal language development. One of the earliest and most sensitive markers for autism spectrum disorder is a 15-month-old child’s inability to point communicatively at objects at a distance. It is theorized that the child cannot imagine that another person would understand what was being indicated; instead, the child indicates wants only by physically touching the desired object or using the adult’s hand as a tool. Research also suggests that differences in sensory processing underlie the social interaction and communication differences present in young children with autism spectrum disorder (2).
Comorbid conditions are common, particularly intellectual disability and learning disorders. Nonfocal neurologic findings include poorly coordinated gait and stereotyped motor movements. Seizures occur in 20 to 40% of these children (particularly those with an IQ < 50).
Довідкові матеріали щодо симптомів та ознак
1. Bradley CC, Boan AD, Cohen AP, Charles JM, Carpenter LA: Reported History of Developmental Regression and Restricted, Repetitive Behaviors in Children with Autism Spectrum Disorders. J Dev Behav Pediatr 37(6):451–456, 2016. doi:10.1097/DBP.0000000000000316
2. Marco EJ, Hinkley LB, Hill SS, Nagarajan SS: Sensory processing in autism: a review of neurophysiologic findings. Pediatr Res 69(5 Pt 2):48R–54R, 2011. doi:10.1203/PDR.0b013e3182130c54
Diagnosis of Autism Spectrum Disorder
Clinical evaluation
Diagnosis of autism spectrum disorder is made clinically based on criteria in the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, Text Revision (DSM-5-TR), and requires evidence of impairment of social interaction and communication and presence of ≥ 2 restricted, repetitive, stereotyped behaviors or interests (as described above under Symptoms and Signs of Autism Spectrum Disorder [1]). Although the manifestations of autism spectrum disorder can vary significantly in scope and severity, previous categorizations such as Asperger syndrome, childhood disintegrative disorder, and pervasive developmental disorder are encompassed under autism spectrum disorder and are no longer distinguished.
Screening tests include the Social Communication Questionnaire (2) for older children and the Modified Checklist for Autism in Toddlers, Revised, with Follow-Up (M-CHAT-R/F) (3).
Formal standard diagnostic tests such as the Autism Diagnostic Observation Schedule-Second Edition (ADOS-2), based on criteria in the DSM-5-TR, are usually given by psychologists or developmental-behavioral pediatricians. Another commonly used tool is the Childhood Autism Rating Scale-Second Edition (CARS2 [4]), which also has a version for testing higher-functioning people. Children with autism spectrum disorder can be difficult to test; they often do better on performance items than verbal items in IQ tests and may show instances of age-appropriate performance despite cognitive limitation in most areas. Nonetheless, reliable diagnosis of autism spectrum disorder is becoming increasingly possible at younger ages. An IQ test given by an experienced examiner often can provide a useful predictor of outcome.
In addition to standardized tests, metabolic and genetic testing is recommended to help identify treatable or inherited disorders, such as an inherited disorder of metabolism and Fragile X syndrome.
Довідкові матеріали щодо діагностики
1. Hyman SL, Levy SE, Myers SM; COUNCIL ON CHILDREN WITH DISABILITIES, SECTION ON DEVELOPMENTAL AND BEHAVIORAL PEDIATRICS: Identification, Evaluation, and Management of Children With Autism Spectrum Disorder. Pediatrics 145(1):e20193447, 2020. doi:10.1542/peds.2019-3447
2. Chandler S, Charman T, Baird G, et al: Validation of the social communication questionnaire in a population cohort of children with autism spectrum disorders. J Am Acad Child Adolesc Psychiatry 46(10):1324-1332, 2007. doi: 10.1097/chi.0b013e31812f7d8d
3. Robins DL, Casagrande K, Barton M, et al: Validation of the modified checklist for Autism in toddlers, revised with follow-up (M-CHAT-R/F). Pediatrics 133(1):37–45, 2014. doi: 10.1542/peds.2013-1813
4. McConachie H, Parr JR, Glod M, et al: Systematic review of tools to measure outcomes for young children with autism spectrum disorder. Health Technol Assess 19(41):1–506, 2015. doi: 10.3310/hta19410
Treatment of Autism Spectrum Disorder
Applied behavior analysis
Speech and language therapy
Sometimes physical and occupational therapy
Pharmacotherapy
Treatment of autism spectrum disorder is usually multidisciplinary, and research shows measurable benefits from intensive, behaviorally based approaches that encourage interaction and meaningful communication. Psychologists and educators typically focus on behavioral analysis and then match behavioral management strategies to specific behavioral problems at home and at school. See also the American Academy of Pediatrics' 2020 clinical report Identification, Evaluation, and Management of Children with Autism Spectrum Disorder.
Applied behavior analysis (ABA) is an approach to therapy in which children are taught specific cognitive, social, or behavioral skills in a stepwise fashion. Small improvements are reinforced and progressively built upon to improve, change, or develop specific behaviors in children who have autism spectrum disorder. These behaviors include social skills, language and communication skills, reading, and academics as well as learned skills such as self-care (eg, showering, grooming), daily-living skills, punctuality, and job competence. This therapy is also used to help children minimize behaviors (eg, aggression) that may interfere with their progress. Applied behavior analysis therapy is tailored to meet the needs of each child and is typically designed and supervised by professionals certified in behavior analysis. In the United States, ABA may be available as part of an Individualized Educational Plan (IEP) through schools and in some states is covered by health insurance. The Developmental, Individual-differences, Relationship-based (DIR®) model, also called Floortime, is another intensive behaviorally based approach. DIR® draws on the child's interests and preferred activities to help build social interaction skills and other skills. At present, there is less evidence to support DIR/Floortime than ABA, but both therapies can be effective.
Speech and language therapy should begin early and use a range of media, including signing, picture exchange, and augmentative communication devices such as those that generate speech based on symbols children select on a tablet or other handheld device, as well as speech. Physical and occupational therapists plan and implement strategies to help affected children compensate for specific deficits in motor function, motor planning, and sensory processing.
Medications may help relieve symptoms. There is evidence that atypical antipsychotic medications (eg, risperidone, aripiprazole) help relieve behavioral problems, such as ritualistic, self-injurious, and aggressive behaviors. Other medications are sometimes used to control specific symptoms, including selective serotonin reuptake inhibitors (SSRIs) for ritualistic behaviors, mood stabilizers (eg, valproic acid) for self-injury and outburst behaviors, and stimulants and other ADHD medications for inattention, impulsivity, and hyperactivity.
Dietary interventions, including some vitamin supplements and a gluten-free and casein-free diet, are not helpful enough to be recommended; however, many families choose to use them, leading to the need to monitor for dietary insufficiencies and excesses. Other complementary and investigational approaches to therapy (eg, facilitated communication, chelation therapy, auditory integration training, hyperbaric oxygen therapy) have not shown efficacy.
Ключові моменти
Children with autism spectrum disorder have some combination of impaired social interaction and communication, repetitive and stereotyped patterns of behavior, and uneven intellectual development often with intellectual disability.
Cause is usually unknown, but there appears to be a genetic component; vaccines are not causative.
Screening tests include the Modified Checklist for Autism in Toddlers, Revised, with Follow-Up (M-CHAT-R/F) and, for older children, the Social Communication Questionnaire.
Formal diagnostic testing is usually done by psychologists or developmental-behavioral pediatricians.
Treatment is usually multidisciplinary, using intensive, behaviorally based approaches that encourage interaction and communication.
Medications (eg, atypical antipsychotics) may help severe behavioral disturbances (eg, self-injury, aggression).
Додаткова інформація
The following English-language resources may be useful. Please note that THE MANUAL is not responsible for the content of these resources.
Modified Checklist for Autism in Toddlers, Revised, with Follow-Up (M-CHAT-R/F)
American Academy of Pediatrics: Identification, Evaluation, and Management of Children With Autism Spectrum Disorder (2020)
Learning Disabilities Association of America (LDA): An organization providing educational, support, and advocacy resources for people with learning disabilities
These organizations provide support, community, and educational resources for people with autism and their caregivers: