- Overview of Esophageal and Swallowing Disorders
- Achalasia
- Distal Esophageal Spasm
- Dysphagia
- Dysphagia Lusoria
- Eosinophilic Esophagitis
- Esophageal Diverticula
- Esophageal Motility Disorders
- Esophageal Rupture
- Esophageal Web
- Gastroesophageal Reflux Disease (GERD)
- Hiatus Hernia
- Infectious Esophageal Disorders
- Lower Esophageal Ring
- Mallory-Weiss Syndrome
- Obstructive Disorders of the Esophagus
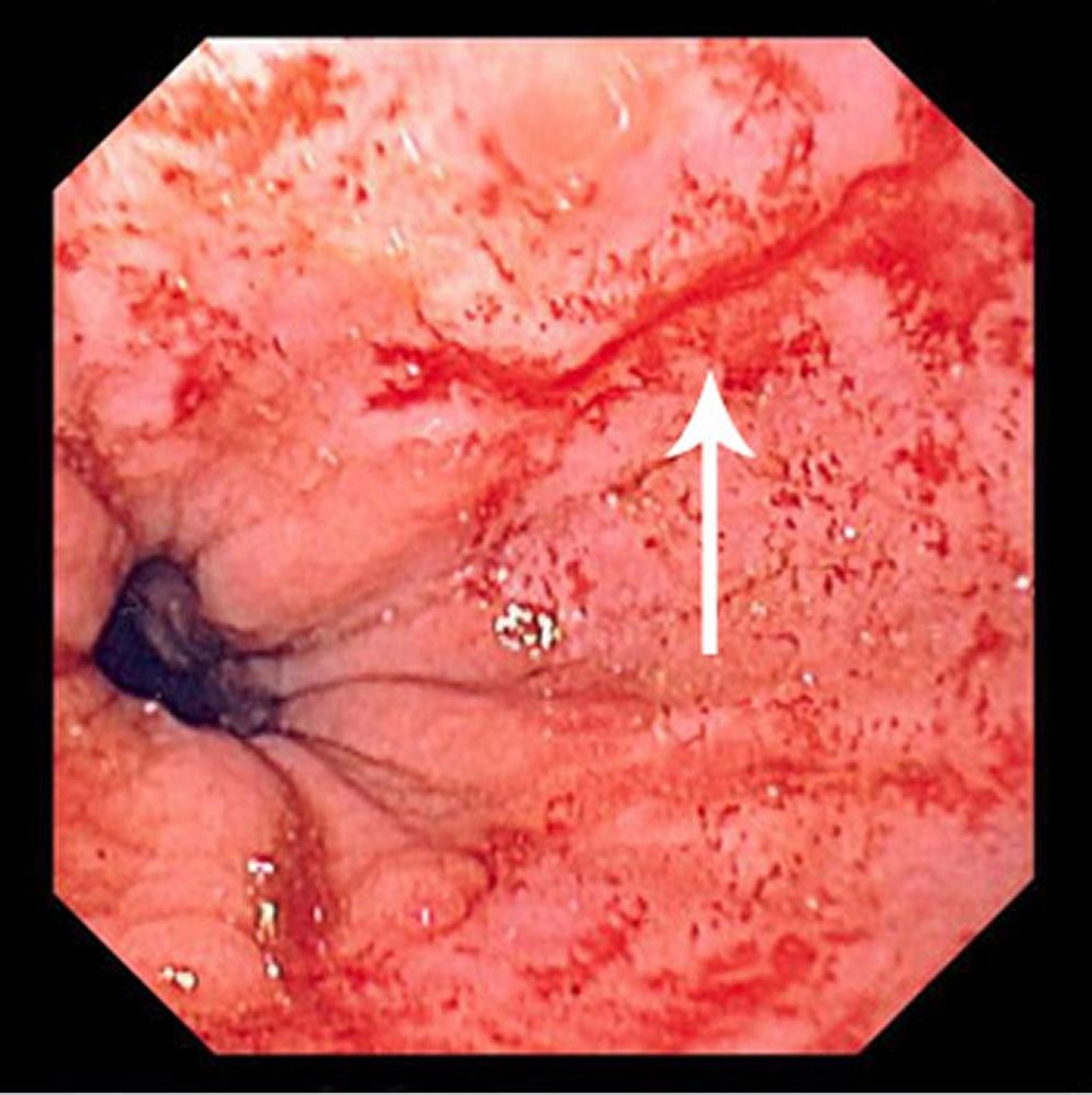
Mallory-Weiss syndrome is a nonpenetrating mucosal laceration of the distal esophagus and proximal stomach caused by vomiting, retching, or hiccuping.
Topic Resources
(See also Overview of Esophageal and Swallowing Disorders.)
Image provided by David M. Martin, MD.
Initially described in patients with alcohol use disorder, Mallory-Weiss syndrome can occur in any patient who vomits forcefully. It is the cause of approximately 5 to 10% of episodes of upper gastrointestinal (GI) hemorrhage (1).
The tear may also be accompanied by pain in the lower chest.
Reference
1. Knoblauch M, Stevka E, Lämmli J, et al: The Mallory-Weiss-syndrome: a clinical study of 20 cases. Endoscopy 8(1):5-9, 1976. doi: 10.1055/s-0028-1098366
Diagnosis of Mallory-Weiss Syndrome
Upper endoscopy
Diagnosis of Mallory-Weiss syndrome is suggested clinically by a typical history of hematemesis occurring after 1 or more episodes of non-bloody vomiting. In such cases, if the amount of bleeding is minimal and the patient is stable, testing may be deferred and some patients can be discharged home.
Otherwise, if history is unclear or bleeding is ongoing, the patient should have standard evaluation for GI bleeding, typically with upper endoscopy and laboratory testing. Upper endoscopy can also be therapeutic because a clip can be placed over the tear to control bleeding.
Treatment of Mallory-Weiss Syndrome
Measures to stop the bleeding
Most episodes of bleeding stop spontaneously; severe bleeding occurs in about 10% of patients, who require significant intervention, such as transfusion or endoscopic hemostasis (by clip placement, injection of ethanol or epinephrine, or by electrocautery). Intra-arterial infusion of vasopressin or therapeutic embolization into the left gastric artery during angiography may also be used to control bleeding. Most episodes of bleeding stop spontaneously; severe bleeding occurs in about 10% of patients, who require significant intervention, such as transfusion or endoscopic hemostasis (by clip placement, injection of ethanol or epinephrine, or by electrocautery). Intra-arterial infusion of vasopressin or therapeutic embolization into the left gastric artery during angiography may also be used to control bleeding.
Surgical repair is rarely required.