Topic Resources
Mirror laryngoscopy, also known as indirect laryngoscopy, is typically done to evaluate symptoms or disorders of the pharynx and larynx. Mirror laryngoscopy is typically used when specialized equipment, such as a rigid or flexible laryngoscope, is unavailable or less convenient (1).
(See also Evaluation of the Patient with Nasal and Pharyngeal Symptoms and Overview of Laryngeal Disorders.)
Indications for Mirror Laryngoscopy
Laryngoscopy may be indicated to evaluate (2):
Chronic cough
Dysphagia
Odynophagia
Hoarseness or change in voice
Dysphonia
Chronic throat pain
Sensation of a lump or foreign body in the throat
Symptoms of aspiration (eg, coughing, choking, and wheezing progressing to fever; chest pain and shortness of breath if there is lung involvement)
Sometimes hemoptysis
In particular, patients at high risk of head and neck cancer (eg, those who smoke heavily or those who regularly use alcohol) may benefit from laryngoscopy, especially if they have had hoarseness, sore throat, or ear pain for > 2 weeks. Patients who have had or require thyroid and parathyroid surgery should also undergo laryngoscopy to assess the function of the recurrent laryngeal nerve and to identify vocal cord paralysis (3).
Laryngoscopy may also be useful to evaluate the airway prior to orotracheal intubation.
Contraindications to Mirror Laryngoscopy
Absolute contraindications
Suspected epiglottitis
In such cases, stimulation of the laryngopharynx may further compromise the airway. If laryngoscopy is essential, it should be done in the controlled setting of an operating room in the presence of a clinician skilled at difficult airway management (including surgical techniques), and ideally performed using direct laryngoscopy (eg, flexible laryngoscopy) rather than mirror laryngoscopy (4).
Relative contraindications
Stridor
Strong gag reflex
Extensive surgery or radiotherapy to the mouth
Anatomical limitations (eg, presence of palatal obturators)
Complications of Mirror Laryngoscopy
Injury to the mucosa, which may cause bleeding
Laryngospasm and airway compromise
The procedure may cause gagging, coughing, and/or vomiting.
Equipment for Mirror Laryngoscopy
Gloves
Protective eyewear
Mask
Tongue depressor
Curved dental mirror
Antifogging solution, warm water (approximately body temperature), or alcohol swab
Headlamp or other external light source that can be used hands-free if possible
Gauze pad 10 cm × 10 cm (4 in × 4 in)
Topical anesthetic spray (eg, lidocaine, benzocaine)Topical anesthetic spray (eg, lidocaine, benzocaine)
Additional Considerations for Mirror Laryngoscopy
Most patients can tolerate mirror laryngoscopy without anesthesia of the oropharynx; however, topical anesthesia may be needed.
If the patient does not tolerate this procedure, flexible laryngoscopy should be done.
Mirror laryngoscopy only provides a limited view of the subglottic larynx and proximal trachea. If pathology is suspected in these regions, use another procedure, such as bronchoscopy.
Relevant Anatomy for Mirror Laryngoscopy
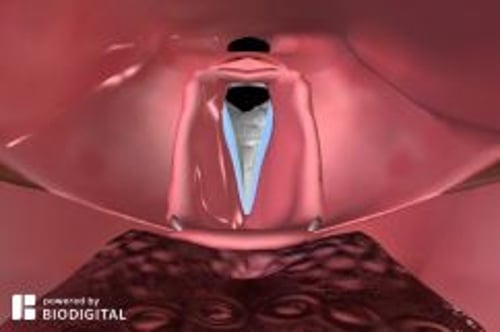
The pharynx includes the nasopharynx, oropharynx, and hypopharynx.
The larynx connects the pharynx to the trachea and is suspended from the hyoid bone. It includes 3 single and 3 paired cartilage structures: single (epiglottis, thyroid, and cricoid) and paired (arytenoid, cuneiform, and corniculate). The larynx extends from the tip of the epiglottis down to the inferior aspect of the cricoid cartilage and includes the vocal folds.
Positioning for Mirror Laryngoscopy
Patient should sit upright with the head against a headrest, and leaning slightly forward, facing the clinician. The proper position is sometimes called the "sniffing position" because the patient appears to be leaning forward as if to smell a flower.
Legs should not be crossed.
Step-by-Step Description of Mirror Laryngoscopy
Direct the external light source toward the patient's oral cavity.
Warm the mirror with warm water (approximately body temperature) to prevent fogging (check to make sure mirror is not too hot). Alternatively, coat the mirror with antifogging solution or alcohol.
Wrap the patient's tongue with gauze and grasp it with your nondominant hand. The gauze will prevent the tongue from slipping and protect it from injury by the lower incisor teeth.
Gently pull on the tongue.
Instruct the patient to breathe deeply through the mouth, to help prevent gagging.
Slide the mirror into the oropharynx without touching the tongue or any mucosa.
Place the back of the mirror against the uvula and gently insert it further until the larynx can be clearly seen.
If gagging occurs, remove the mirror and spray the posterior oropharynx with a topical anesthetic.
Move the mirror gently and as little as possible to inspect the base of the tongue, valleculae, epiglottis, piriform sinuses, arytenoids, false and true vocal cords, and if possible to visualize, the larynx below the vocal cords.
Rotate the mirror from side to side between the thumb and forefinger to bring lateral structures into view.
Fully inspect the vocal cords.
Instruct the patient to say "eeee," which will contract the vocal cords, thereby permitting assessment of their function.
Aftercare for Mirror Laryngoscopy
Instruct the patient to avoid eating and drinking for at least 20 minutes after the procedure to avoid aspiration due to residual laryngopharyngeal anesthesia.
Warnings and Common Errors for Mirror Laryngoscopy
Failure to align the light source as closely as possible with the line of sight
Failure to warm the mirror, because a cold mirror will fog
Failure to maintain an adequate hold of the patient's tongue to keep it retracted
Allowing the patient to lean back, which will prevent full visualization
Positioning the mirror at the wrong angle to see the larynx
Tips and Tricks for Mirror Laryngoscopy
To avoid neck strain, raise the patient's chair so that the mirror can be held close to the examiner's eye level.
Use one finger of the hand holding the mirror to elevate the upper lip.
Touching the uvula alone should not elicit the gag reflex, but avoid touching the back or sides of the throat, which can.
References
1. Collins SR. Direct and indirect laryngoscopy: equipment and techniques. Respir Care. 2014;59(6):850-864. doi:10.4187/respcare.03033
2. Hull JH, Backer V, Gibson PG, et al. Laryngeal Dysfunction: Assessment and Management for the Clinician. Am J Respir Crit Care Med. 2016;194(9):1062-1072. doi:10.1164/rccm.201606-1249CI
3. Sinclair CF, Bumpous JM, Haugen BR, et al. Laryngeal examination in thyroid and parathyroid surgery: An American Head and Neck Society consensus statement: AHNS Consensus Statement. Head Neck. 2016;38(6):811-819. doi:10.1002/hed.24409
4. Moellman JJ, Bernstein JA, Lindsell C, et al. A consensus parameter for the evaluation and management of angioedema in the emergency department. Acad Emerg Med. 2014;21(4):469-484. doi:10.1111/acem.12341