Ultrasound-guided cannulation of the subclavian vein uses real-time (dynamic) ultrasound to guide venipuncture and a guidewire (Seldinger technique) to thread a central venous catheter through the subclavian vein and into the superior vena cava. Two approaches (infraclavicular and supraclavicular) are used; the infraclavicular approach is described here.
Using ultrasound guidance to approach the subclavian vein infraclavicularly requires that the axillary vein (distal continuance of the subclavian vein) is imaged and cannulated because the clavicle blocks ultrasound imaging of the proximal vein. Cannulating the axillary vein may be difficult to do with or without ultrasound guidance, and ultrasound guidance, if available, is mandatory.
(See also Vascular Access, Central Venous Catheterization, and How To Do Subclavian Vein Cannulation.)
Indications for Infraclavicular Subclavian Vein Cannulation, US-Guided
Secure or long-term venous access that is not available using other sites
Inability to obtain peripheral venous access or intraosseous infusion
IV infusion of fluids and medications for patients in cardiac arrest
IV infusion of medications that may be irritating to veins when administered peripherally (eg, high-concentration fluids, chemotherapy, vasopressors, parenteral nutrition)
IV infusion of high flows or large fluid volumes beyond what is possible using peripheral venous catheters
Hemodynamic monitoring (eg, central venous pressure, central venous oxyhemoglobin saturation, cardiac pressures via pulmonary artery catheters)
Transvenous cardiac pacing or pulmonary arterial monitoring (Swan-Ganz catheter)†
* The subclavian vein may be less preferred for stiff catheters (because of difficulty achieving the sharp turn into the superior van cava) or large-bore hemodialysis catheters (which can cause venous stenosis that renders the ipsilateral arm unsuitable for arteriovenous shunt placement).
† For transvenous cardiac pacing and pulmonary arterial monitoring, a right internal jugular cannulation or a left subclavian vein cannulation typically is preferred.
A subclavian central venous catheter (CVC) is preferred for long-term venous access in patients who are not confined to bed (eg, ambulatory patients needing parenteral nutrition, antibiotics, or chemotherapy).
Contraindications to Infraclavicular Subclavian Vein Cannulation, US-Guided
Absolute contraindications
Untrained or inexperienced ultrasound operator
Unsuitable axillary/subclavian vein, thrombosed (incompressible) or inaccessible as seen by ultrasound
Fracture of the clavicle or proximal ribs
Local infection at the insertion site
Antibiotic-impregnated catheter in a patient with an allergy to the specific antibiotic
Relative contraindications
Unilateral lung disease: Cannulate ipsilaterally.
Local anatomic distortion, traumatic or congenital, without pneumothorax: Cannulate contralaterally.
Coagulopathy, including thrombocytopenia or anticoagulant medications (including antiplatelet medications)*
Gross obesity: Because the axillary vein lies deep and the brachial plexus is nearby, cannulate the axillary vein only in patients who are thin.
Malignant superior vena cava syndrome
Severe cardiorespiratory insufficiency or increased intracranial or intraocular pressure: These patients will be compromised by Trendelenburg (head down) positioning.
History of prior catheterization of the subclavian vein: Prior catheterization may have resulted in scar tissue formation making catheter placement more difficult.
Uncooperative patient: Sedate if necessary.
Left bundle branch block: A guidewire or catheter in the right ventricle can induce complete heart block.
* Anticoagulant medications (eg, for atrial fibrillation) increase the risk of bleeding with subclavian vein cannulation, but this risk must be balanced against the increased risk of thrombosis (eg, stroke) if anticoagulation is reversed. Discuss any contemplated reversal with the clinician managing the patient's anticoagulation and then with the patient. A femoral line may be preferred.
Complications of Infraclavicular Subclavian Vein Cannulation, US-Guided
(See also Complications of central venous catheterization.)
Potential complications include
Pneumothorax (increased risk because apical pleura [especially on left side] is close to needle insertion path)
Arterial puncture
Hematoma (increased risk because clavicle impedes application of external pressure to stop subclavian arterial or venous bleeding)
Damage to the vein
Hemothorax
Air embolism
Thoracic duct puncture
Catheter misplacement* (eg, internal jugular vein, thoracic duct)
Arrhythmias or atrial perforation, typically caused by guidewire or catheter
Nerve damage
Infection
Thrombosis (due to the catheter itself)
* Rare complications due to catheter misplacement include arterial catheterization, hydrothorax, hydromediastinum, and damage to the tricuspid valve.
Use of ultrasound decreases the risk of arterial puncture and possibly pneumothorax.
Guidewire or catheter embolism also rarely occurs.
To reduce the risk of venous thrombosis and central line-associated bloodstream infection (CLABSI), CVCs should be removed as soon as they are no longer needed.
Equipment for Infraclavicular Subclavian Vein Cannulation, US-Guided
Sterile procedure, barrier protection
Antiseptic solution (eg, chlorhexidine-alcohol, chlorhexidine, povidone-iodine, alcohol)Antiseptic solution (eg, chlorhexidine-alcohol, chlorhexidine, povidone-iodine, alcohol)
Large sterile drapes, towels
Sterile hats, masks, gowns, gloves
Face shields
Ultrasound guidance
Ultrasound machine with a high-frequency (eg, 5 to 10 MHz), linear array probe (transducer)
Ultrasound gel, nonsterile and sterile
Sterile probe cover to ensheathe probe and probe cord, sterile rubber bands (alternatively, the probe may be placed within a sterile glove and the cord wrapped within a sterile drape)
Seldinger (catheter-over-guidewire) technique
Cardiac monitor
Local anesthetic (eg, 1% lidocaine without epinephrine, approximately 5 mL)Local anesthetic (eg, 1% lidocaine without epinephrine, approximately 5 mL)
Small anesthetic needle (eg, 25 to 27 gauge, 3 cm [approximately 1 inch] long)
Large anesthetic/finder* needle (22 gauge, 4 cm [approximately 1.5 inches] long)
Introducer needle (eg, thin-walled, 18 or 16 gauge, with internally beveled hub, 6 cm [approximately 2.5 inches] long)
3- and 5-mL syringes (use slip-tip syringes for the finder and introducer needles)
Guidewire, J-tipped
Scalpel (#11 blade)
Dilator
Central venous catheter (adult: 8 French or larger, minimum length for axillary/subclavian catheter is 20 cm [approximately 8 inches] for right side and 24 cm [approximately 9.5 inches] for left side)
Sterile gauze (eg, 10 × 10 cm [4 × 4 inch] squares)
Sterile saline for flushing catheter port or ports
Nonabsorbable nylon or silk suture (eg, 3-0 or 4-0)
Chlorhexidine patch, transparent occlusive dressingChlorhexidine patch, transparent occlusive dressing
* A finder needle is a thinner needle used for locating the vein before inserting the introducer needle. It is usually not needed for ultrasound-guided cannulation.
The external diameter of the CVC should be less than or equal to one-third of the internal diameter of the vein (as measured by ultrasound) to reduce the risk of thrombosis.
Having 1 or 2 assistants is helpful.
Additional Considerations for Infraclavicular Subclavian Vein Cannulation, US-Guided
The short-axis (cross-sectional, transverse) ultrasound view is easy to obtain and is the better view for identifying veins and arteries and their orientation to each other. Identifying a needle tip in cross section requires some skill because the needle appears as an echogenic (ie, white) dot and the tip can be distinguished only by the dot's disappearance and reappearance as the needle tip traverses back and forth across the imaging plane. The short-axis view typically is used to determine a suitable venous impalement site and to guide steeply angled (eg, ≥ 45°) needle insertions.
The long-axis (longitudinal, in-plane) ultrasound view is technically more difficult to obtain (must keep probe, vein, and needle in one plane), but it shows the needle longitudinally, so the entire needle—including the tip—can be imaged continuously as it approaches and enters the vein; this continuous view helps avoid aberrant placement. The long-axis view is helpful when the angle of needle insertion is shallow (eg, in axillary/subclavian cannulations) and to affirm proper longitudinal needle alignment during short-axis insertions.
Cannulation attempts sometimes fail. Do not exceed 2 or 3 attempts (which increases the risk of complications), and use new equipment with each attempt (ie, do not re-use needles, catheters, or other equipment because they may have become blocked with tissue or blood).
During cardiopulmonary arrest, or even low blood pressure and hypoxia, arterial blood may be dark and not pulsatile and may be mistaken for venous blood.
If the subclavian artery is errantly cannulated by either the tissue dilator or the CVC, leave the dilator or catheter in place and obtain surgical consultation for possible surgical removal.
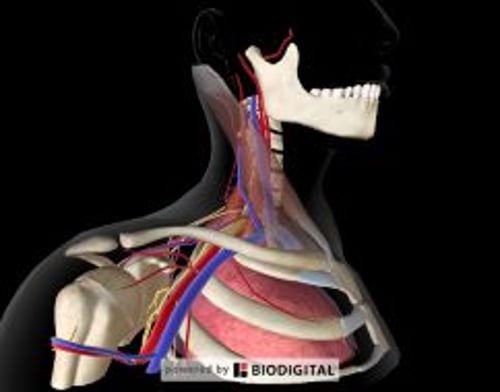
Relevant Anatomy for Infraclavicular Subclavian Vein Cannulation, US-Guided
The subclavian vein is the proximal continuation of the axillary vein and extends medially from the lateral edge of the first rib to the brachiocephalic (innominate) vein.
Because ultrasound waves do not penetrate bone, the axillary vein (distal subclavian vein) is imaged inferior to the lateral clavicle (for the infraclavicular approach).
The axillary vein extends laterally from the first rib to the teres major muscle, where it becomes the brachial vein. Normal anatomic variation in the orientation of the axillary vein and artery is great, so ultrasound guidance is of particular value (and is recommended as mandatory) in this region.
The axillary vessels are best identified by using a short-axis (cross-section) view in the area inferior to the distal clavicle, where the vessels are most superficial and have their largest diameter.
A long-axis (longitudinal) view and shallow angle of needle insertion are useful for the axillary vein cannulation to avoid impaling the pleura.
The skin insertion site is influenced by both the imaging and the dimensions of the transducer tip (ie, the skin insertion site for long-axis ultrasound guidance may be several centimeters distal to that for short-axis ultrasound guidance).
Right subclavian cannulation, versus left, is sometimes preferred because it avoids the thoracic duct and because the right pleural apex is lower than the left. Left cannulation is sometimes preferred because it affords a direct, less angular path into the superior vena cava, with less chance of misdirected catheterization of the internal jugular vein.
Positioning for Infraclavicular Subclavian Vein Cannulation, US-Guided
Raise the bed to a comfortable height for you (ie, so you may stand straight while doing the procedure).
Place the patient supine or in Trendelenburg position (bed tilted with the head down 10 to 20°) to distend the axillary vein and prevent air embolism.
The arm may comfortably rest at the patient's side, and the head is kept neutral.
Stand at the side of the bed.
Step-by-Step Description of Infraclavicular Subclavian Vein Cannulation, US-Guided
Check that the ultrasound machine is configured and functioning correctly: Ensure that the screen image you are seeing correlates to the spatial orientation of the probe as you are holding and moving it. The side mark on the probe tip corresponds to the marker dot on the ultrasound screen. Adjust the screen settings and probe position if needed to attain an accurate left-right orientation.
Do a nonsterile ultrasound inspection (ie, using an uncovered probe and nonsterile gel) and determine whether the vein is suitable for cannulation. Use a short-axis (cross-sectional) view. Examine the area inferior to the distal clavicle. Blood vessels are hypoechoic (appear black on the ultrasound screen). Veins are generally larger, thin-walled, and ovoid (rather than thick-walled and round) and are more easily compressed (by gentle pressure on overlying skin) than their paired arteries. The size of the axillary vein varies with respiration and is increased by the Trendelenburg position and the Valsalva maneuver.
Venous thrombosis may appear as an echogenicity (gray irregularity) in the lumen but often is diagnosed because the thrombosed vein is incompressible. Thrombosis disqualifies the vein as a suitable cannulation site.
Cannulate a central vein at a site of optimal short-axis imaging (ie, large-diameter cross section of the vein, with no overlying artery).
Attach the cardiac monitor to the patient and turn it on.
Prepare the equipment
Place sterile equipment on sterilely covered equipment trays.
Use appropriate personal protective equipment.
Draw the local anesthetic into a syringe.
Attach the introducer needle to a 5-mL syringe with 1 to 2 mL of sterile saline in it. Align the bevel of the needle with the volume markings on the syringe.
Pre-flush all lines of the CVC with 3 to 5 mL of sterile saline and then close the ports with caps or syringes.
When flushing a central line, use a 10-mL syringe (or one of equal or greater diameter) and do not push too hard to avoid rupturing the line.
Prepare the sterile field
Swab a broad area of skin with antiseptic solution, encompassing the entire clavicular and shoulder area. Also include the side of the neck and anterior chest to below the ipsilateral nipple so you can immediately switch to internal jugular cannulation should the axillary/subclavian vein cannulation fail.
Allow the antiseptic solution to dry for at least 1 minute.
Place sterile towels around the site.
Place large sterile drapes (eg, a full-body drape) to establish a large sterile field.
Put on sterile mask and hat.
Put on sterile gown and gloves.
Place a sterile cover over the ultrasound probe
Direct your assistant (nonsterile) to coat the probe tip with nonsterile ultrasound gel and then hold the probe, with the tip pointing up, just outside the sterile field.
Insert your gloved dominant hand into the sterile probe cover.
Grasp the tip of the probe with your dominant hand (now covered by the probe cover).
Use your gloved nondominant hand to unroll the sterile cover over the probe and completely down the cord. Do not touch the uncovered cord nor allow it to touch the sterile field as you unroll the cover.
Pull the cover tightly over the probe tip to eliminate all air bubbles and ensure that the probe tip remains coated with ultrasound gel.
Wrap sterile rubber bands around the probe to secure the cover in place.
The covered probe may now rest on the sterile drapes.
Anesthetize the cannulation site
Apply sterile ultrasound gel to the covered probe tip.
Use long-axis ultrasound guidance for axillary/subclavian vein cannulation for both the local anesthetic and the introducer needle insertions:
First, use short-axis ultrasound guidance to attain an optimal cross-sectional image of the axillary vein inferior to the distal clavicle. Press lightly with the probe tip to avoid distorting the image size and shape of the vein.
Next, rotate the probe 90° to attain the long-axis (in-plane, longitudinal) view of the axillary vein, placing the medial end of the probe over the site of the optimally imaged short-axis view. Move the probe as needed to attain the widest image of the vein, which occurs when the probe overlies the vein's longitudinal axis. Press lightly with the probe tip so the vein remains centered under the tip and does not roll to the side.
Keep the probe in this spot.
When using long-axis ultrasound guidance, insert procedural needles (local anesthetic and introducer needles) into the skin at a point just distal to the distal end of the probe, and initially advance the needle into the skin at a shallow angle (approximately 30°) beneath the long axis of the probe. Slightly adjust probe and needle as needed to keep both in-plane. As you advance, adjust the insertion angle so that the needle meets the vein at the proximal end of the probe. Keep gentle negative pressure on the syringe plunger as you advance.
Place a wheal of anesthetic just lateral to the lateral end of the probe tip and then, under ultrasound guidance, inject anesthetic into the skin and soft tissues superficial to the vein along a shallow angle passing medially underneath the probe. Adjust the insertion angle as necessary to keep the needle safely distant from the vein.
Insert the introducer needle using ultrasound guidance
Continue to use long-axis ultrasound guidance (as described above for the local anesthetic injection).
Insert the introducer needle (with needle bevel aligned along the insertion path).
Maintain longitudinal visualization of the needle and the vein as you advance by making slight adjustments to the lateral direction of the needle and orientation of the probe.
If the needle strays from the vein, it will appear to shorten. Adjust the lateral direction of the needle to image its entire length. If the needle tip is approaching the vein too steeply, withdraw the needle a bit, decrease the angle of insertion, and re-advance.
As the needle tip approaches the vein, temper your speed and angle of insertion so the needle enters with as much control as possible. The superficial wall of the vein will indent when the needle tip encounters it. The needle then pops through the wall to enter the lumen, accompanied by a flash of dark red blood in the barrel of the syringe.
Hold the syringe motionless in this spot and visualize the tip of the needle at all times. Displacement is common, and even a slight movement may displace the needle tip from the vein.
Assess the blood return
Continue to hold the syringe motionless.
Securely grasp the needle hub and also hold it motionless.
Remove the syringe from the needle hub and briefly let blood flow out to confirm that the blood is venous (ie, dark red and flowing but not pulsatile). Then immediately cover the hub with your thumb to stop the blood flow and prevent air embolism.
However, if the blood is bright red and pulsatile (arterial), terminate the procedure. Remove the needle and use gauze squares for 10 minutes to hold external pressure on the area and to help prevent bleeding and hematoma.
Insert the guidewire
Carefully rotate the introducer syringe such that the bevel of the needle now faces inferiorly (ie, away from the internal jugular vein and toward the heart).
Insert the J-curved end of the guidewire into the introducer needle, with the J curve facing inferiorly (ie, in the same direction as the needle bevel).
Advance the guidewire through the needle and into the vein. You may use ultrasound guidance (either short- or long-axis) to verify the guidewire entering the vein. Do not force the guidewire; it should slide smoothly. Advance the guidewire 20 to approximately 23 cm or until ectopic heartbeats occur (withdraw from this point until ectopy stops).
If you feel any resistance as you advance the guidewire, stop advancing it. Try to gently withdraw the guidewire slightly, rotate it slightly, and then re-advance it, or try to gently withdraw the guidewire entirely, reestablish the needle tip within the vein (confirmed by venous blood return), and then reinsert the guidewire.
However, if you feel any resistance as you withdraw the guidewire, terminate the procedure and withdraw the needle and guidewire together as a unit (to prevent the needle tip from shearing through the guidewire within the patient). Then use gauze squares for 10 minutes to hold external pressure on the area and to help prevent bleeding and hematoma.
Once the guidewire has been inserted, continue to hold it securely in place with one hand and maintain control of it throughout the remainder of the procedure to avoid wire embolism.
Remove the introducer needle (after successful guidewire insertion)
First, securely hold the guidewire distal to the needle and pull the needle from the skin.
Then, securely hold the guidewire at the skin surface and slide the needle down the remaining length of the guidewire to remove the needle.
Widen the insertion tract
Extend the skin insertion site: Using the scalpel, make a small stab incision (approximately 4 mm) into the skin insertion site, avoiding contact with the guidewire, to enlarge the site and allow it to accommodate the larger diameters of the tissue dilator and the catheter.
Advance the tissue dilator over the guidewire: First, grasp the guidewire at the skin and slide the dilator down the length of the wire to the skin. Then grasp the guidewire just distal to the dilator, hold the dilator near the skin surface, and use a corkscrew motion as needed to stepwise insert dilator to pass through the wall of the vein. Maintain your grasp on the guidewire at all times during the insertion.
Remove the dilator: First, securely hold the guidewire distal to the dilator and pull the dilator from the skin. When the guidewire is visible at the skin surface, completely remove the dilator by sliding it down the remaining length of the guidewire.
Maintain your grasp on the guidewire at the skin surface.
Place the catheter
Advance the catheter over the guidewire to the skin surface: Hold the guidewire fixed at the skin surface, thread the catheter tip over the distal end of the guidewire, and slide the catheter down to the skin surface. The distal end of the guidewire should now be protruding from the port hub.
If the distal end of the guidewire is not protruding from the port hub, incrementally advance the guidewire outward from the skin surface while holding the catheter tip close to the surface until the guidewire protrudes.
Continue to advance the catheter into the vein: Grasp and control the guidewire where it protrudes from the hub. Hold the catheter near its tip and insert the tip through the skin. Then, in increments of several centimeters and using a corkscrew motion as necessary, stepwise advance the entire length of the catheter. If ectopic heartbeats occur, slowly withdraw the catheter until ectopy stops.
Use ultrasound to verify the intravenous placement of the catheter.
Maintain your grasp on both the guidewire and the catheter.
Remove the guidewire: Withdraw the guidewire while holding the catheter securely in place at the skin surface.
Flush each catheter port with saline: First, draw any air from the line and confirm venous blood flow into the hub. Then, using a 10-mL syringe (or one of equal or greater diameter) and without using excessive force, push 20 mL of saline into the line to clear it.
Dress the site
If the patient is awake or minimally sedated, use 1% lidocaine to anesthetize the skin at the planned suture locations.If the patient is awake or minimally sedated, use 1% lidocaine to anesthetize the skin at the planned suture locations.
Place a chlorhexidine-impregnated disk on the skin at the catheter insertion point. Place a chlorhexidine-impregnated disk on the skin at the catheter insertion point.
Suture the skin to the mounting clip on the catheter.
To prevent pulling on the insertion site, suture the catheter at a second site so that a curved or looped segment of catheter lies between the 2 sites.
Apply a sterile occlusive dressing. Transparent membrane dressings are commonly used.
Aftercare for Infraclavicular Subclavian Vein Cannulation, US-Guided
Before using the catheter, do chest radiography to confirm that the tip of a subclavian (or jugular) venous catheter lies in the superior vena cava near its junction with the right atrium (the catheter can be advanced or retracted if not in the appropriate position) and to confirm that pneumothorax has not occurred.
The red arrow points to the tip of a left subclavian venous port catheter (placed appropriately in the lower superior vena cava).
Warnings and Common Errors for Infraclavicular Subclavian Vein Cannulation, US-Guided
The tip of a CVC must never lie in the right atrium because the atrium is thin-walled and easily perforated.
Cardiac ectopy may be induced by a guidewire or catheter in the right atrium or ventricle.
Never lose grasp of the guidewire.
During cardiopulmonary arrest, or even low blood pressure and hypoxia, arterial blood may be dark and not pulsatile and may be mistaken for venous blood.
Placing a pillow under the patient's back to facilitate subclavian line placement may hinder correct placement by narrowing the space between the clavicle and first rib.
To help prevent air embolism, CVCs should be inserted (and removed) with the vascular cannulation site positioned dependant to the heart.