Abdominal aortic branch occlusion is blockage or narrowing of one of the large arteries in the abdomen that come off of the aorta.
Branches of the aorta can be blocked (occluded) due to atherosclerosis, abnormal growth of muscle in the artery's wall (fibromuscular dysplasia), blood clots, or other disorders.
Blockage causes symptoms related to the lack of blood flow, including pain, in the area the artery serves.
Imaging tests are used to make the diagnosis.
Treatment is with removal of a blood clot, angioplasty, or sometimes surgical bypass grafting.
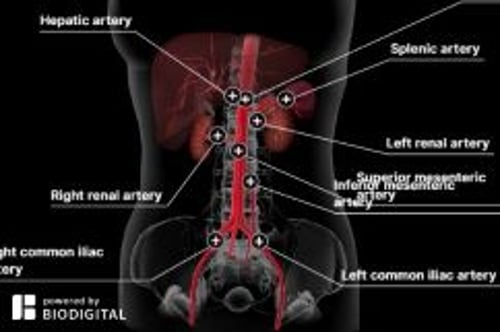
The aorta is the largest artery of the body. It receives oxygen-rich blood from the heart and distributes it to the body through smaller arteries that branch off of it. The abdominal aorta is the part of the aorta that passes through the abdominal cavity. Important branches of the abdominal aorta include the arteries that supply blood to the
Intestine (celiac artery and superior and inferior mesenteric arteries)
Kidneys (renal arteries)
Legs (iliac arteries)
Blockage of the arteries that branch off of the aorta may develop suddenly or slowly.
Sudden blockage (acute occlusion) of branches of the abdominal aorta may result from a blood clot that has developed in the artery or traveled into it from elsewhere (embolism), or because the layers of the artery suddenly separated (dissection).
Slowly developing blockage of branches of the abdominal aorta may result from hardening of the arteries (atherosclerosis), in which deposits of cholesterol and other fatty materials (atheromas or atherosclerotic plaques) develop in the walls of arteries, abnormal growth of muscle in the artery's wall (fibromuscular dysplasia), or compression of the artery by a growing abdominal tumor.
Similar blockage can develop in arteries of the legs or, less commonly, the arms (see Occlusive Peripheral Arterial Disease).
Symptoms of Abdominal Aortic Branch Occlusion
Sudden blockage shuts off blood flow, which causes immediate, severe pain. Pain may be in the abdomen, back, or legs, depending on which artery is blocked. Organ failure and tissue death (necrosis) occur within hours unless blood flow is restored.
Symptoms of slowly developing blockage vary depending on which artery is involved and the severity of the blockage.
Lower aorta and common iliac arteries
Sudden blockage of the lower aorta where it divides into the common iliac arteries causes both legs to suddenly become painful, pale, and cold. No pulse can be felt in the legs, which may become numb. Sudden blockage of an iliac artery causes symptoms in only one leg. These symptoms indicate a medical emergency.
Gradual narrowing of the lower aorta or of the common iliac arteries can cause cramping and pain when walking (intermittent claudication) that affects the buttocks and thighs of both legs. The legs may also feel cold or appear pale, although they usually appear normal. Chronic occlusion can also cause erectile dysfunction. This combination of claudication and erectile dysfunction is sometimes called Leriche syndrome.
Renal arteries
Sudden, complete blockage of one of the renal arteries, which supply the kidneys, may cause a sudden pain in the side, and the urine may become bloody. These symptoms indicate a medical emergency.
Gradual, moderate narrowing of one or both renal arteries may not cause symptoms or affect kidney function. Rarely, more complete narrowing of one or both renal arteries contributes to the development of kidney failure and high blood pressure (a disorder called renovascular hypertension). Less than 5% of people with high blood pressure have renovascular hypertension. However, renovascular hypertension can be hard to control.
Superior mesenteric artery
Sudden, complete blockage of the superior mesenteric artery causes severe abdominal pain, nausea, and vomiting. These symptoms indicate a medical emergency.
Initially, most people with a sudden blockage of the superior mesenteric artery vomit and feel an urgent need to have a bowel movement. They may become seriously ill and have severe abdominal pain because the superior mesenteric artery supplies a large part of the intestine. The abdomen may feel tender when a doctor presses on it, but the severe abdominal pain is usually more prominent than the tenderness, which is widespread and vague. The abdomen may be slightly swollen (distended). Through a stethoscope, a doctor initially hears fewer bowel sounds in the abdomen than normal. Later, no bowel sounds can be heard. The stool initially contains small amounts of blood but soon looks bloody. Blood pressure falls, and shock may result as areas of the intestine die (called necrosis or gangrene).
Gradual narrowing of the superior mesenteric artery typically causes pain about 30 to 60 minutes after each meal, because the intestine requires more blood during digestion. The pain is steady, severe, and usually centered at the navel. This pain makes people afraid to eat, so they may lose considerable weight. Because the blood supply to the intestine is reduced, nutrients may be poorly absorbed into the bloodstream, contributing to the weight loss. People who have pain after they eat may also have nausea, vomiting, constipation, or diarrhea.
Hepatic and splenic arteries
Blockage of the hepatic artery, which supplies the liver, or the splenic artery, which supplies the spleen, is usually not as dangerous as blockage of the major arteries that supply the intestine. However, parts of the liver or spleen may be damaged. People with hepatic artery occlusion may have no symptoms or may have abdominal pain, fevers and chills, nausea, vomiting, and yellowing of the skin and whites of the eyes (jaundice).
People with splenic artery occlusion may have no symptoms or may have abdominal pain, fevers, and chills.
Diagnosis of Abdominal Aortic Branch Occlusion
Imaging tests
Doctors usually suspect the diagnosis on the basis of the person's symptoms and findings during the physical examination. Imaging tests such as ultrasound, computed tomography (CT) angiography, magnetic resonance angiography, or traditional angiography are used to confirm the diagnosis.
Usually, angiography, an invasive procedure in which a flexible plastic catheter is inserted into one of the large arteries in the upper thigh, is done only when surgery or angioplasty (opening up a blockage by inflating a small balloon within the artery) is required. In such cases, its purpose is to provide doctors with clear images of the affected arteries before surgery or angioplasty is done. Rarely, angiography is needed to determine whether surgery or angioplasty is possible. In angiography, a contrast agent that can be seen on radiographic images is injected into an artery via the flexible plastic catheter. The contrast agent shows an outline of the inside of the artery when x-ray studies are done. Thus angiography can show the precise diameter of the artery and is more accurate than ultrasound in detecting some blockages.
Most medical centers do angiography using a less invasive method such as computed tomography (CT angiography) or magnetic resonance imaging (called magnetic resonance angiography, or MRA). Rather than requiring an insertion of a flexible catheter into a major artery, these tests use small amounts of a radiographic contrast agent that are injected into the bloodstream by vein using a standard intravenous catheter in the arm.
Treatment of Abdominal Aortic Branch Occlusion
Restoration of blood flow by angioplasty or removal of blood clot
Acute occlusion is a surgical emergency requiring removal of the blood clot (embolectomy), angioplasty, or some other procedure (such as injecting medications to break up the clot or doing emergency surgical bypass) to restore blood flow to the affected area.
Lower aorta and common iliac arteries
For sudden, complete blockage of the lower aorta and common iliac arteries, removal of the clot is done immediately. Clot removal is done using a catheter inserted into an artery, which is then used to dislodge or vacuum out the clot, or by making an incision in the artery during open surgery and manually removing the clot.
Renal arteries
Angioplasty with removal of a blood clot, insertion of a stent, or surgery is done for sudden, complete blockage of a renal artery. If done promptly, the procedure can restore blood flow and kidney function.
In angioplasty, a catheter with a balloon at its tip is inserted into the narrowed part of the artery and then the balloon is inflated to clear the blockage. Sometimes an expandable metal mesh tube (stent) is placed at the site of the blockage to keep the blood vessel open. Some stents contain medications that are slowly released (drug-eluting stents) and prevent recurrence of the blockage. If chronic blockage causes symptoms, surgery or angioplasty may be needed. Antiplatelet therapy is given postoperatively.
Medical treatment is needed for gradual, moderate blockage of a renal artery as long as blood pressure is controlled and blood tests indicate that the kidneys are functioning adequately. If renovascular hypertension develops, antihypertensive medications are used. Often, at least three antihypertensives are needed. Angiotensin-converting enzyme (ACE) inhibitors are particularly useful. Kidney function must be monitored when ACE inhibitors are used. If high blood pressure persists and is severe or if kidney function is deteriorating, doctors may do angioplasty or bypass surgery to restore blood flow to the kidney.
Superior mesenteric artery
When the superior mesenteric artery is suddenly and completely blocked, only immediate intervention can restore the blood supply fast enough to save the person's life. Doctors may use angioplasty with stent placement, bypass surgery, embolectomy, or treatment with medication. Often, to save time, doctors send people straight to surgery rather than do diagnostic tests first. During surgery, doctors may remove or bypass the blockage. If the intestine is damaged and does not improve after the blood supply is restored, the affected piece of intestine may have to be removed.
Medications that dissolve clots (thrombolysis) or widen (dilate) the arteries may be given during the procedure when the diagnosis of blockage is made by angiography. These medications are given directly into the artery and may open the blockage. This procedure may avoid the need for surgery. Whether a person survives and whether the intestine can be saved depend on how fast the blood supply is restored.
NitroglycerinNitroglycerin may relieve the abdominal pain if the superior mesenteric artery has gradually narrowed, but angioplasty or surgery is still needed to widen the artery.
Hepatic and splenic arteries
Surgery is needed to clear a blockage of the hepatic or splenic artery.